How to Manage Asthma in Winter :- If you live on the East Coast and have asthma, you probably already know how the cold affects your asthma symptoms. The daytime highs in Connecticut are often around 30°F, making winters there somewhat cold.
The best strategy to avoid flare-ups and maintain well-controlled asthma is to understand how cold weather affects asthma. Wintertime can make asthma management a bit tough. Asthma sufferers find the winter months in Manchester and the surrounding areas to be especially challenging.
People who have asthma are prone to get flare-ups during the cold. We offer practical advice on managing your asthma over the winter months in this post.
Understanding cold weather and asthma symptoms
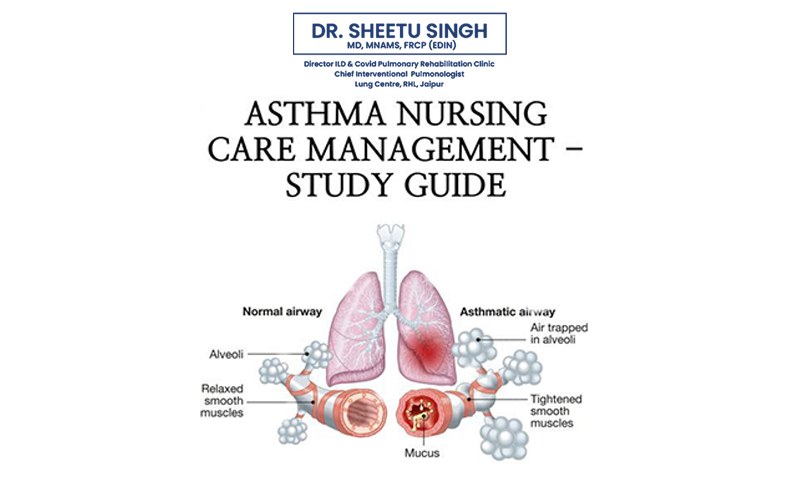
People who have asthma have sensitive bronchial tubes that are stimulated by cold air, among other things. The lining of your airways may get irritated when the outside temperature drops and you breathe in cold air, leading to symptoms like wheezing, coughing, and shortness of breath.
Winter is a more likely season to cause flare-ups for asthmatic individuals than other seasons. Symptoms of cold air might arise, particularly in dry and windy situations. The more severe your asthma is, the more likely it is that exposure to cold air can aggravate your symptoms.
Limit indoor triggers
Asthma sufferers face not only the actual cold but also the added challenge of spending more time indoors throughout the winter. Mold and dust mites are two common indoor asthma causes for many people.
Your asthma may worsen if you spend more time indoors where allergens are present. If you suffer from indoor allergies, take preventative measures in advance of winter, such as installing HEPA filters to reduce allergens in your house or, if you have a dust mite allergy, covering your pillows and mattress with dust mite coverings.
Keep warm
Winter is not the appropriate season for those with asthma to go outside with inadequate clothing. Asthma flare-ups can be prevented by staying warm. Depending on the outside temperature, it makes sense to bundle up. Wear a warm coat, gloves, a hat, and a scarf during the winter.
Wearing a mask or scarf over your mouth and nose can also be helpful. By doing this, you reduce the chance of irritating your airway by helping to warm the chilly air as you inhale.
Avoid mouth breathing
Some people have a propensity of breathing via their mouths. But when it’s chilly outside, it’s crucial that you breathe through your nose if you have asthma. When it’s chilly outside, breathing through your lips lets the cold air rush into your lungs, which might set off an asthma attack.
The nasal cavity’s structures warm and humidify the air as it passes through when you breathe in through your nostrils. Your airway irritation risk is reduced since the air is warmer when it enters your lungs.
Follow a winter asthma management plan
In order to effectively manage your asthma during the colder months, preparation is essential. Together with your provider, develop a winter asthma plan.
It’s wise to arrange routine checks in addition to adhering to your winter asthma plan. This allows your doctor the chance to keep an eye on you, make sure your medication is effective, and make sure your asthma is under control for the winter.
Call us to make an appointment with Dr. Sheetu Singh or make an online reservation right now to find out more about the best ways to manage asthma in the winter.
What can you do if you’re having an asthma attack?
Consult your doctor and the asthma action plan you created if you begin to wheeze or feel out of breath.
In the event that your symptoms are so bad that you are unable to talk, take your quick-acting medication and get help right away. It could be necessary to keep you under observation until your breathing becomes steady.
Other general recommendations on what to do in the event of an asthma attack are as follows:
- Utilizing a quick-acting rescue inhaler, take two to six puffs. Your airways should be cleared by the medication, making breathing simpler for you.
- Nebulizers can potentially be a viable substitute for inhalers. A nebulizer is a device that creates a tiny mist for you to breathe in while taking your medication.
- After taking your inhaler for a few puffs, if your symptoms aren’t getting better but you still need to wait 20 minutes before taking another dose.
- Dial your doctor as soon as you feel better. For a day or two, you might need to continue taking your quick-acting medication every few hours.
Takeaway for people with Asthma
After taking your medication and getting inside out of the cold, your asthma episode should go away.
You might need to visit your doctor to have your asthma action plan reviewed if your symptoms don’t get better or if they seem to grow worse every time you’re outside in the cold. They might advise you to switch medications or think of alternative ways to manage your illness.