We examine the top 10 infectious diseases for 2023 in this post. Numerous various bacteria, ranging from a mild cold virus to pulmonary TB, can induce coughing and fever.
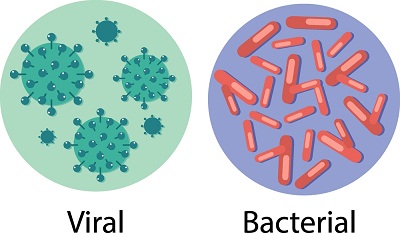
What is an infection?
An infection occurs when a microorganism- such as fungi, bacteria or virus enters a person’s body and causes harm. The immune system can frequently prevent these viruses from multiplying within the body. The microorganism relies on the host’s body to survive, procreate, and colonize. These infectious, quickly reproducing microscopic pathogens.
How can infections spread?
They can spread through a variety of channels, such as:-
- Skin contact.
- Transfer of body fluids
- Contact with faces
- Ingesting contaminated water or food
- airborne particles or droplets being inhaled
- Touching a surface that has been touched by a person who is infected with the disease.
So, here are 10 significant prevalent infections in 2023.
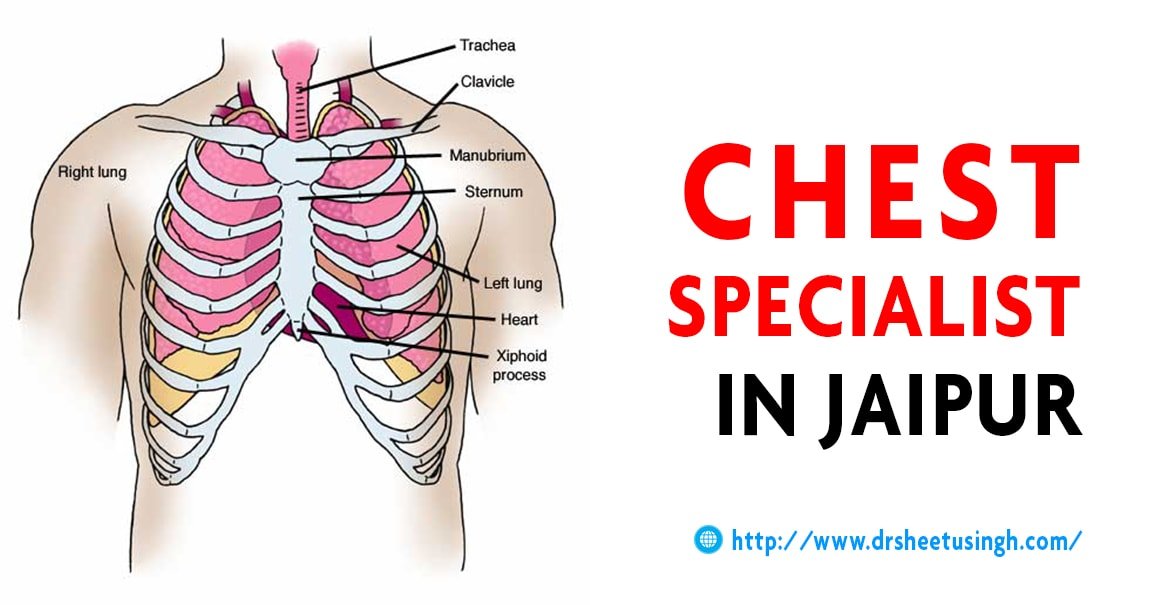
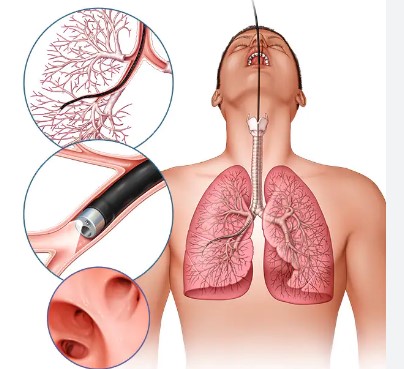
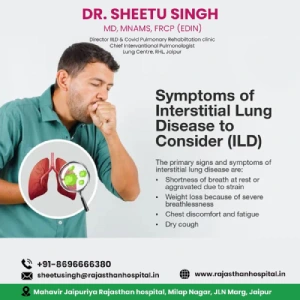
1- Bronchitis: An inflamed bronchi is known as bronchitis. This produces sputum and a cough. They are typically brought on by a virus and will heal on their own. It is an upper respiratory tract infection (URTI) that is most frequently seen. When treating bronchitis, Dr. Sheetu Singh takes a thorough, patient-centered approach. She emphasizes on giving each bronchitis patient individualized care using her broad medical knowledge and sympathetic personality. Your immune system creates swelling and mucus buildup in your airways when they are stimulated.
2- Common colds and influenza: Colds and influenza (flu) are both contagious respiratory infections, although they are brought on by various viruses. Different viruses, such as rhinoviruses, parainfluenza, and seasonal coronaviruses, can cause the common cold, however, only influenza viruses can cause the flu. Colds are usually milder than flu. Compared to those who have the flu, cold sufferers are more likely to have a runny or congested nose. In most cases, significant health issues like bacterial infections, pneumonia, or hospitalization are not brought on by colds. Flu can have serious associated complications.
3- Conjunctivitis: Conjunctivitis, also referred to as “pink (or red) eye,” is an inflammation of the eye and eyelid lining. The eye whites seem pink and could be discharged with something sticky. There are three main kinds of causes for conjunctivitis:-
- Infective conjunctivitis- infection caused by a virus or bacteria. This illness may spread quickly.
- Allergic conjunctivitis: An allergic response to something such as pollen or dust mites.
- Irritant conjunctivitis- Objects that can irritate the conjunctiva come into touch with the eye, such as stray eyelashes or chlorinated water, or shampoo.
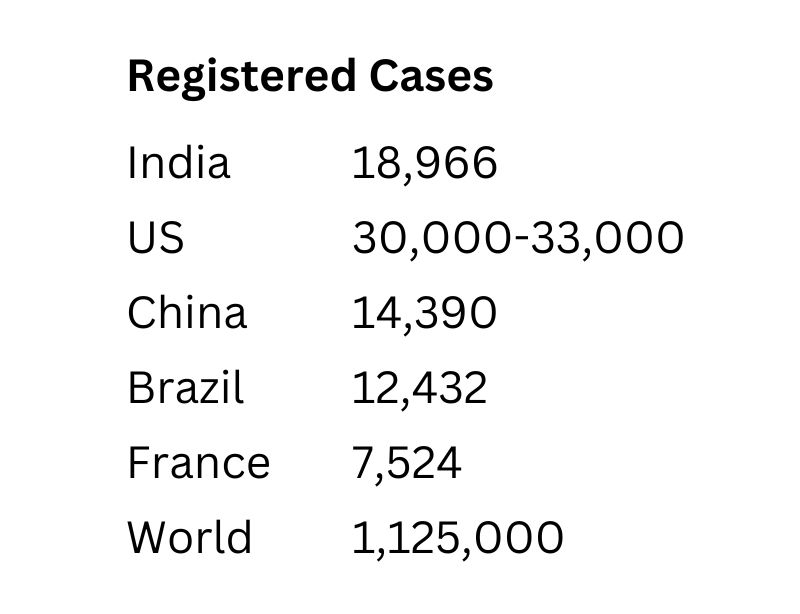
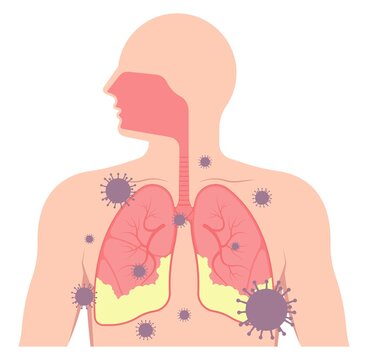
4- COVID-19: The SARS-cov-2 virus is the infectious agent that causes coronavirus illness. Most virus-infected people will develop a mild to severe respiratory illness, but they will recover without the need for special treatment. Serious illness is more likely to affect the elderly and those with underlying medical illnesses including cancer, diabetes, cardiovascular disease, or persistent respiratory issues. Early symptoms of COVID-19 may include a loss of smell or taste. Other symptoms may include:-
- Muscle aches
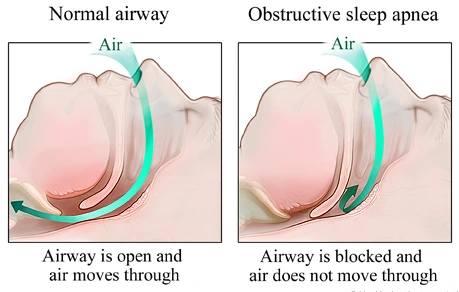
- Shortness of breath or difficulty breathing
- Sore throat
- Runny nose
- Headache
- Rash
- Chest pain
5- Gastroenteritis: Gastroenteritis is a very common condition that causes vomiting and diarrhea. It is usually caused by a viral tummy bug or bacteria that can be related to food. It affects people of all ages but is simply common in young children. A virus known as rotavirus is responsible for the majority of illnesses in children. An intestinal infection known as viral gastroenteritis has symptoms such as watery diarrhea, stomach cramps, nausea, and occasionally fever.
6- HIV/AIDS: The immune system of the body is attacked by the human immunodeficiency virus. Acquired immunodeficiency syndrome may result from untreated HIV. There is currently no effective treatment available. When someone contracts HIV, they are permanently infected and can be controlled with proper medical care. HIV is caused by a virus. It may also spread from mother to child during pregnancy, childbirth, and breastfeeding. It can also spread through sexual contact, drug use or sharing of needles during illicit injections and contact with infected blood.
7- Malaria: Malaria is caused by plasmodium parasites. Humans are the only significant repository for four Plasmodium species—Plasmodium falciparum, Plasmodium vivax, Plasmodium Ovale, and Plasmodium Malariae—all of which cause disease in people. It can manifest in a variety of forms, from a minor chronic sickness to an acute illness that poses a serious threat to life. The majority of malaria deaths are caused by one or more major complications like breathing problems, cerebral malaria, anemia, organ failure or low blood sugar.
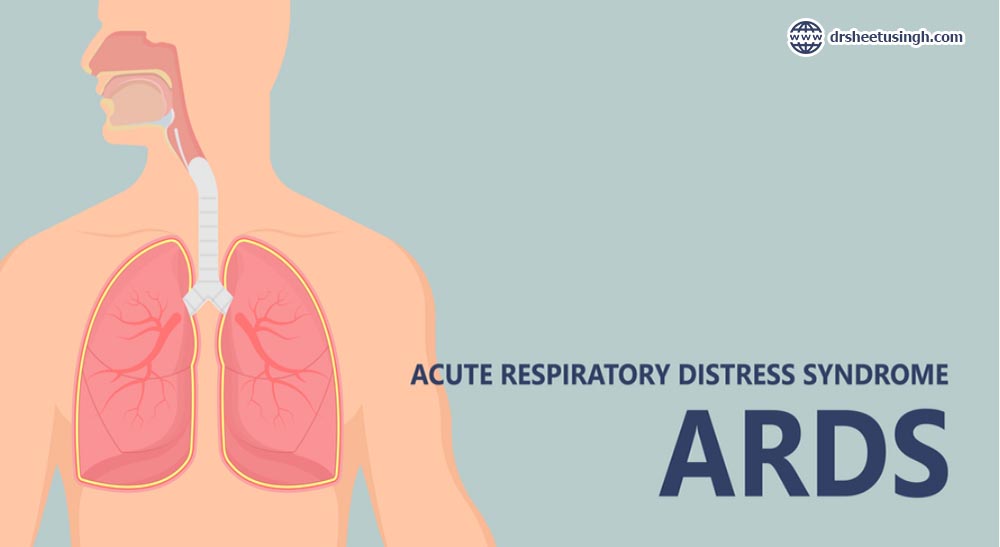
8- Pneumonia: Pneumonia is an infection of one or both of the lungs caused by viruses, bacteria or fungi. It is a dangerous infection when bacteria and other liquids fill the air sacs. It can be identified if there are typical symptoms linked with new chest X-ray shadowing. Signs and symptoms of pneumonia may include cough, fatigue, fever, sweating, nausea, vomiting chest pain or shortness of breath. There are two main types:-
- One or more lung chambers can become infected with lobar pneumonia.
- One or more lung chambers can become infected with lobar pneumonia.
9- Sore throat: Sore throat is usually caused by viruses like flu, cold or COVID-19. They may occasionally be brought on by bacteria. Most people recover without any kind of treatment. A sore throat can also be caused by:-
- Pharyngitis
- Laryngitis
- Tonsillitis
- Glandular fever
10- Tuberculosis (TB): Tuberculosis is a highly infectious bacterial disease that mostly affects the lungs. It can affect any part of the body including the nervous system, glands and bones. TB can spread when a person with sneezes, illness coughs or sings. This may release microscopic droplets containing the germs into the atmosphere. There are numerous symptoms associated with active TB, the majority of which are respiratory. Dr. Virendra Singh treats tuberculosis with a combination of expertise, compassion and innovation. Dr. Virendra Singh represents excellence in tuberculosis treatment via his commitment to improving tuberculosis care and his sympathetic approach. The symptoms include:
- Cough
- Fever
- Unexplained fatigue
- Blood in sputum
- Night sweats
- Chest pain
- Appetite loss
- Weight loss