Managing Winter Asthma and Allergies: Winters are harsh on those, who are struggling with asthma and prone to various allergies. Such people struggle a lot during cold weather due to their narrow respiratory airways and other complications. But now you don’t worry. We understand this is going to be tough on you, but this blog will help you a bit and make your life in winters a bit easier.
Here in the details mentioned below, we will explain to the readers that “How can they manage asthma and allergies during the winter season?” So let’s start catching up with the very much required information.
Caution: Before you get into the info, make sure if you face some extreme medical challenges, then you better consult with the doctor. Consult with “Dr. Sheetu Singh” to make your condition better and help you lead a better lifestyle afterwards.
Is Asthma Triggered from the Cold Air?
When the asthmatic or the allergic person breathes in cold air, it causes issues with the internal muscles and makes them spasm when they are also trying to keep open up. Cold air can make asthma worse by irritating the airways, causing coughing, wheezing, and trouble breathing. People with asthma also struggle more in cold, dry air, especially when it’s windy. The colder and drier the air, the more likely it is to trigger asthma symptoms. Especially those who are much critically triggered with asthma have more problems during such seasons. So, if you have asthma, it’s important to stay warm and avoid being outside in very cold weather. Make sure you better take care of yourself when there is windy air outside.
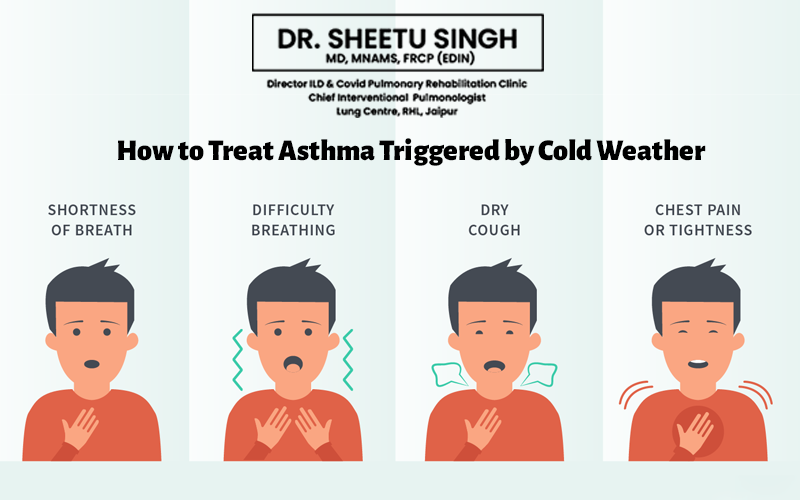
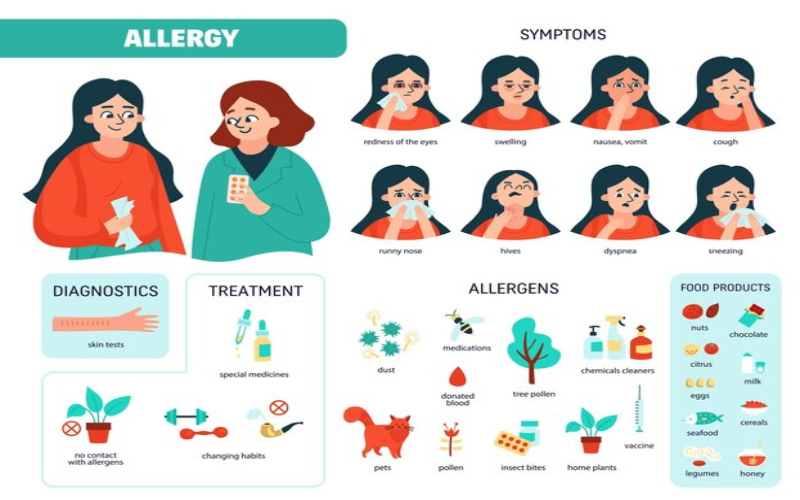
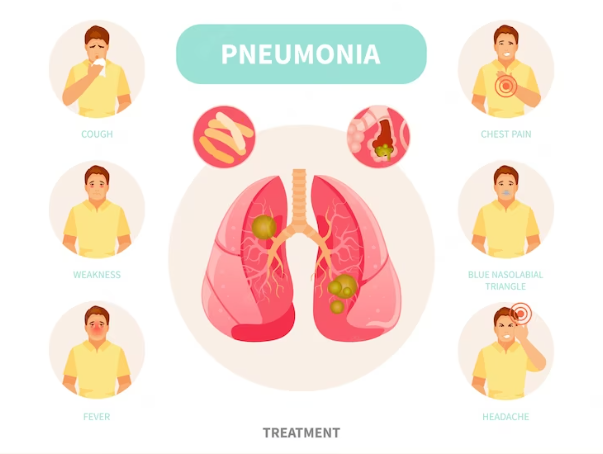
What are the Symptoms of Cold-Weather Induced Asthma?
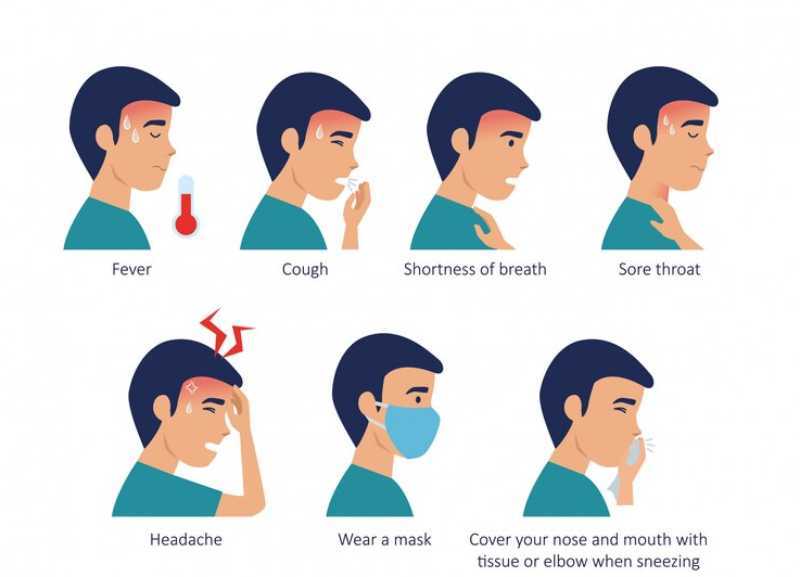
Symptoms of asthma triggered by cold weather are similar to those caused by other few reasons. These may include:
- Coughing: This can be either dry or accompanied by phlegm.
- Wheezing: It is often heard when the person is exhaling.
- Shortness of breath: Difficulty breathing deeply during cold winter weather.
- Chest tightness: A feeling of constriction in the chest area.
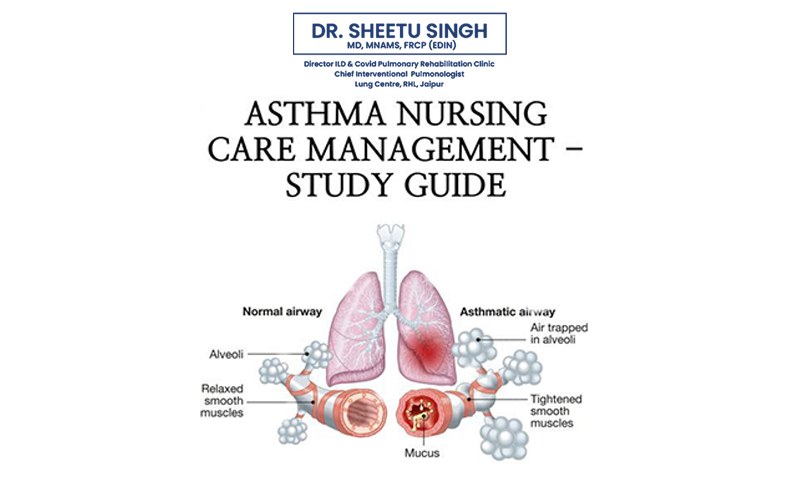
Why is Cold Weather Hard on People with Asthma?
Winter brings a range of weather or climatic changes, including cold and dry air, snow, rain, and gusty winds, which can impact individuals even in regions with milder climates. These conditions, coupled with fluctuations in air pressure, are known triggers for health issues. Rainy and windy weather can agitate mold spores, while changes in barometric pressure can lead to sinusitis, both of which may provoke asthma flare-ups.
Furthermore, the winter season sees a surge in illnesses such as colds, flu, and viruses. These infections can exacerbate asthma symptoms by thickening mucus in the bronchial tubes, making breathing more challenging. Consequently, individuals may experience heightened symptoms or asthma flare-ups.
Moreover, during colder months, people tend to spend more time indoors with windows shut and heating systems active. This prolonged indoor exposure increases the likelihood of encountering indoor allergens, irritants, and respiratory viruses. Common triggers include dust, mold, pet dander, and cigarette smoke, all of which can potentially induce asthma flare-ups. Therefore, it’s essential for individuals with asthma to be mindful of these factors and take necessary precautions to manage their condition effectively during the winter season.
Cold Weather can Cause Asthma Attack
If cold air tends to trigger your asthma, it’s crucial to be cautious during chilly weather to avoid asthma attacks. Refer to your Asthma Action Plan for guidance on managing asthma in cold conditions, and don’t hesitate to seek medical help if your symptoms worsen.
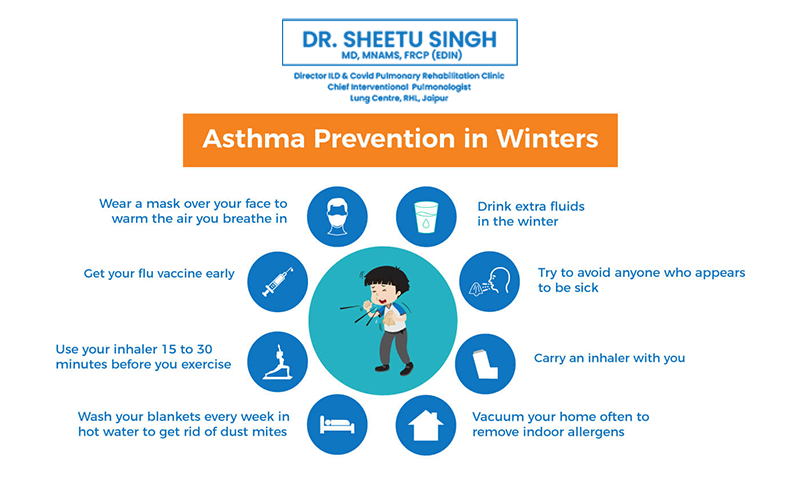
To protect yourself from asthma flare-ups caused by cold air:
Wrap a scarf around your mouth and nose to warm the air before breathing it in.
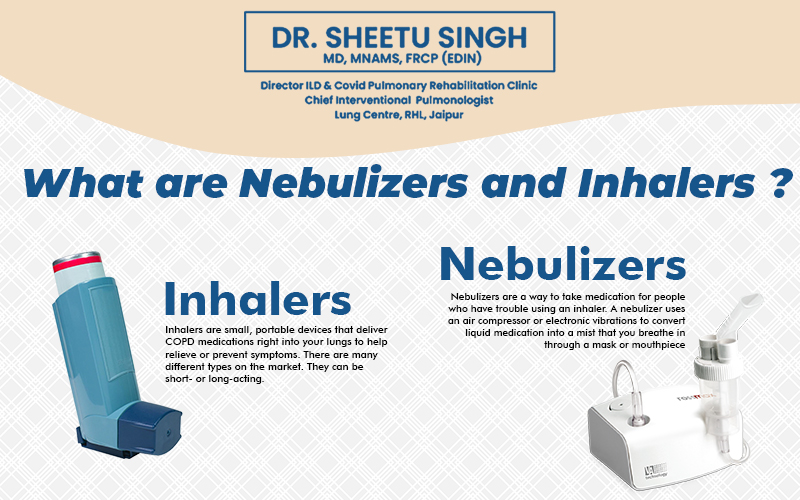
Keep a short-acting albuterol inhaler handy and use it at the first sign of symptoms to prevent your asthma from getting worse.
Try to stay indoors whenever possible to breathe warmer air, but ensure the indoor environment is free from allergens and irritants.
If you frequently experience asthma symptoms in cold weather, discuss with your doctor about a long-term treatment plan tailored to your needs.
How to Handle Asthma during Winters?
There are a few things you need to take care of. Read the pointers mentioned below and know what best to do for taking care of yourself:
- Exercise indoors instead of outside.
- Wrap a scarf around your mouth and nose in cold weather.
- Use humidifiers at home, and keep them clean to prevent mold.
- Wash your hands often with soap or sanitizer to avoid winter illnesses.
- Avoid touching your face and eyes to prevent spreading germs.
- Get flu and COVID-19 vaccines as recommended.
- Have an Asthma Action Plan ready for flare-ups.
- If you’re allergic to pet dander, limit time with pets and keep your bedroom pet-free.
- Control dust mites and mold by keeping your home cool and dry.
- Clean or replace filters in your heating and cooling systems regularly to maintain good indoor air quality.
Conclusion
Asthma and Allergies, these both can make a person feel so depressive and irritating. We understand the concern and know how much the patients are struggling because of these. But don’t worry, because we can help you out. Hope the information we have shared above was enough for you. Besides sharing this much information, we would like to recommend consulting with Dr. Sheetu Singh. She is the best pulmonologist in Rajasthan, who has the experience and practice enough to guide best.